News, ideas & inspiration from industry leaders

Veterinary Shortage Update: Q&A on VPA
The Veterinary Professional Associate model is a viable solution to the veterinary shortage—and there’s science to back it up
The shortage of veterinarians in the United States is real. We first blogged about it in 2021, when we reported on the idea of creating a new class of professionals—the mid-level Veterinary Professional Associate (VPA)—as one potential solution. While there has been much support for this idea, not everyone is on board. But there’s good news: just-published research, The Veterinary Professional Associate Financial Model: Shelter Practice, may change some minds. The research explores the viability of VPA model, with the results of the study extremely encouraging. We recently spoke with James W. Lloyd, DVM, PhD, one of the study’s authors, to find out more.
The Association: What is the current situation in sheltering that the VPA provides a solution for?
Dr. Lloyd: The shortage of veterinarians in the United States is limiting access to, and increasing the price of, pet healthcare. As a consequence, pets are more likely to be surrendered to shelters either with an existing adverse health condition, or because of an inability to schedule and/or afford veterinary care. This situation increases the demands on the shelter community’s veterinary workforce, which is already shorthanded because of the insufficient numbers of veterinarians. It is extremely difficult for the current population of shelter veterinarians to meet the volume of medical and surgical needs, and the VPA will help to extend the veterinarians’ reach.
The Association: Briefly explain the methodology used to conduct your research.
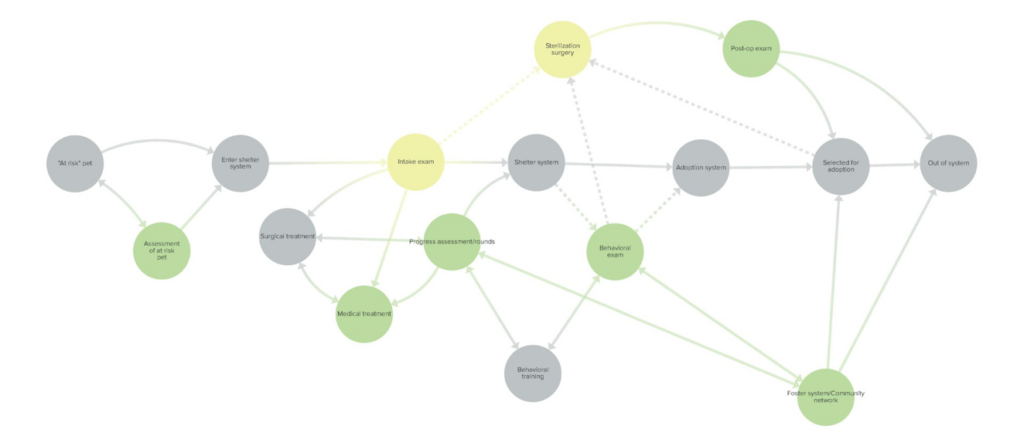
Dr. Lloyd: To determine the potential impact of a VPA, we started with an extensive round of interviews with thought leaders from across the veterinary profession and the shelter community. Using that information, we then created a systems model incorporating site-specific Shelter Animals Count (SAC) data to simulate the flow of animals and associated workloads in a particular shelter both with and without a VPA.
The Association: Can you share high-level outcomes?
Dr. Lloyd: Under our model assumptions, adding one full-time equivalent (FTE) VPA markedly increased capacity/throughput and improved financial performance in a shelter environment. Specifically,
- Total live outcomes per year increased,
- Estimated operating cost per live outcome decreased, and
- Days in shelter decreased
These findings suggest that VPAs could be a viable solution to help address the capacity issues in veterinary medicine. Similar to successful implementations of physician assistants and nurse practitioners in human medicine, VPAs may enhance capacity in a nonprofit shelter practice, improve patient outcomes and animal welfare, and improve shelter financial performance.
The Association: What are your recommendations for the field? How can shelters apply your research to their everyday operations?
Dr. Lloyd: Shelter leadership should carefully consider bottlenecks in their own operations to determine the potential impact of a VPA. If the medical and/or surgical capacity of the current veterinary workforce is found to be a key constraint, then a VPA should be seriously considered.
The Association: What does the future of sheltering look like with the VPA?
Dr. Lloyd: As the key roles, responsibilities, and capabilities of VPAs begin to emerge and be well-recognized, shelter healthcare teams stand to become more efficient and effective, leading to enhanced capacity, improved patient outcomes and animal welfare, and improved shelter financial performance.
The Association: Knowing that there are concerns in the field regarding the VPA role, what insights might you have for those who are not yet on board?
Dr. Lloyd: As currently envisioned, the VPA would work under the supervision of a veterinarian. Ideally, the veterinarian would be able to delegate many of the more routine tasks to the VPA, thus freeing up the veterinarian to allocate a greater proportion of their time to more complex medical and surgical cases. Further, the VPA roles and responsibilities would complement – not replace – contributions of others on the healthcare team.